Feeling short of breath can have a big impact on your life. But there are people who can support you and things you can do yourself that can help you to manage breathlessness.
Understanding breathing
Most of the time we do not think about our breathing. We just do it automatically. But if you have an illness that causes breathlessness, it may become an effort.
Knowing a bit about how your lungs work can help you to understand why you feel breathless.
How we breathe
Our bodies need oxygen all the time. If our muscles do not get enough oxygen, we become breathless. The medical word for breathlessness is dyspnoea (also spelled dyspnea).
When we breathe in (inhale), air enters through our mouth or nose and goes into the windpipe (trachea). This makes our chest and lungs expand. When we breathe out (exhale), our lungs get smaller again.
A large muscle under the lungs called the diaphragm (dye-uh-fram) helps get air into the lungs and allows them to expand. We also have muscles between the ribs (intercostal muscles) that help the chest to expand and let air into our lungs. This is called intercostal breathing.
When we're relaxed and breathing is easy, we use the diaphragm and intercostal muscles to breathe. If you're finding it harder to breathe, muscles in the shoulders and chest can help too but they get tired quickly.
How our bodies breathe is call the respiratory system.
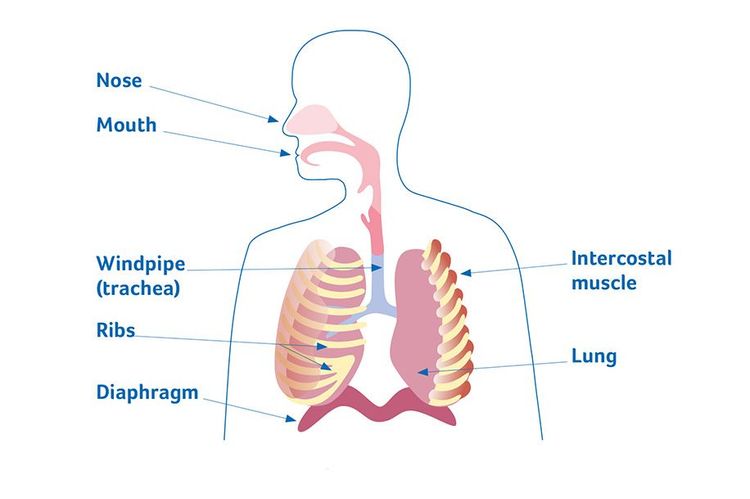
The respiratory system.
What is breathlessness (also called dyspnoea)?
Breathlessness, or shortness of breath, is an uncomfortable feeling of difficulty with breathing. It's normal to feel breathless at times (for example, after running for a bus). But breathlessness can also be caused by illness.
Even if you're having the right treatment, some people may still feel breathless. Breathlessness that develops over weeks or months like this is called long-term (chronic) breathlessness.
People's experience of breathlessness can be different. Some people feel breathless all the time (constant breathlessness). For other people, it may come and go (called episodic breathlessness). You might feel more breathless when you're doing an activity, or if you're feeling anxious − or you might not know why you're feeling breathless.
How breathlessness can affect day-to-day life
Breathlessness can affect every part of your life and it can be difficult to deal with. You may feel breathless walking, getting dressed, climbing stairs, having a shower or doing housework.
If breathlessness is making it more difficult to do things you usually do, you might need to ask friends, family members and professionals for support.
Breathlessness can feel frightening. You might feel worried or panicky when you feel breathless (see What can you do to manage breathlessness? below).
What causes breathlessness?
You can develop breathlessness if any part of your respiratory system is not working properly.
Speak to your doctor or nurse if you feel breathless. They can find out what's causing it and recommend the best ways to manage it. If there's a reversible cause for the breathlessness, like an infection, they can treat this.
Sometimes people still experience breathlessness after an illness has been treated. Tell your doctor or nurse if this happens to you as there are treatments that can help.
What can you do to manage breathlessness?
There are lots of things you can do that can help with breathlessness. You can try the suggestions on this page. And you may want to ask your doctor or nurse if there's a breathlessness service in your local area.
We also have a free booklet with breathing techniques, medicines and other things that can help.
Try different breathing positions
Sitting, standing or lying in certain positions can make it easier to fill your lungs with air when you breathe in. We explain these positions below. Not every position works for everyone, but you can try them out and see what works best for you.
-
Sit upright in a chair with your back against the back of the chair and rest your hands on your thighs.
-
Sit on a chair leaning forward with your forearms resting on your thighs.
-
Sit or stand leaning forward with your arms resting on a ledge, for example a windowsill or table.
-
Lean back against a wall with your feet a comfortable distance from the wall and slightly apart. Relax your shoulders and let your arms hang down by your sides or rest them in your pockets.
-
If you're in bed, try to lean back against a few pillows so you're sitting upright. Or you can lie on your side with pillows under your head and shoulders. Make sure the top pillow supports your head and neck. A V-shaped pillow can be helpful.
Once you're in one of these positions you can try breathing control techniques.
Breathing techniques
There are different techniques that can help control your breathing at times when you feel out of breath. You might find that some of them work better than others. You can try them by yourself – of if you need any extra help, ask your physiotherapist, doctor or nurse.
Try breathing control
Breathing control means using techniques to breathe gently, using as little effort as possible. They can help when you are short of breath or feeling anxious. These techniques can help let more air into your lungs and allow you to feel more in control of your breathing.
Pursed-lip breathing
Pursed-lip breathing is something you can try at any time to help you control your breathing. You can also use it while you're doing something that makes you feel breathless to help you feel less short of breath.
This is how to do pursed-lip breathing:
- Get into a comfortable position for your breathing.
- Breathe in gently through your nose.
- Purse your lips as if you were going to whistle.
- Blow out with your lips pursed when you breathe out.
- Do this gently for as long as it feels comfortable.
- Do not force the air out of your lungs.
You might want to practice it first when you're not feeling breathless, so you know how to do it if you do feel out of breath.
Blow as you go
This breathing control technique helps you to breathe more easily while doing activities. You can use it while you're doing something that makes you breathless.
Blow as you go means:
- Taking a breath in just before you do something.
- Then breathing out while you're doing it. It can be helpful to use pursed-lips when you blow out.
This can be useful for an activity that feels like an effort. For example:
- stretching your arms above your head to reach for something
- reaching or bending down
- lifting something heavy
- climbing stairs
- standing up.
Manage anxiety
If you feel anxious or start to feel panicky when you get breathless, it can help to try some relaxation techniques to help control your breathing.
Rectangular breathing can help to get your breathing under control when you're feeling anxious. You need to concentrate on this exercise so it helps to distract you from feeling worried.
Imagine a rectangle. Or you can look at a rectangle that's in the room, such as a TV screen or picture frame.
- Breathe in and imagine going up one side of the rectangle.
- Breathe out and imagine going along the top of the rectangle.
- Breathe in and imagine going down the other side of the rectangle.
- Breathe out and imagine going along the bottom of the rectangle.
Keep breathing in and out in this way until your breathing feels under control.
As you get used to doing it, try blowing out for longer than you're breathing in.

Rectangular breathing.
Anxiety support
If you're finding it difficult to cope with anxiety, it can help to talk to someone you trust. This could be a friend, family member or your doctor or nurse.
You can also contact our Support Line for free on 0800 090 2309 or email us at support@mariecurie.org.uk for practical information and emotional support.
Your doctor or nurse can prescribe medicines to help, and they can refer you to a different professional for more support. A counsellor or psychologist can help you understand and work through your feelings.
Counselling is a talking therapy that is sometimes free at hospices, hospitals or GP surgeries. If this is something you want to try, ask your doctor or nurse. They can let you know what talking therapies are available locally and can help you decide which treatment is best for you. For more information about free counselling services, speak to your GP.
You may also be able to get private counselling, which you would need to pay for. For more information, ask your doctor or visit the British Association of Counselling and Psychotherapy website (see link below) to find a qualified counsellor near you.
Find ways to relax
Finding ways to relax may help you manage breathlessness and anxiety. Try to find time for relaxation each day. You might find it helps to do breathing exercises, listen to music or an audiobook, spend time outside, have a bath or you might want to try meditating.
Making the most of the energy you have
Following the five Ps − prioritising, planning ahead, pacing, positioning and permission – is a way to make the most of your energy. It can mean you don't feel breathless as quickly when you're doing an activity. It can be particularly helpful for people who have fatigue as well as breathlessness.
Make changes to how and what you're eating
If you get breathless when you're eating, you may find it helps to try these things:
- Take your time while you're eating.
- Try softer, moist foods like soups, smoothies and pureed foods that are easier to chew and swallow.
- Sit down to eat and do not eat while you're on the move.
- Try not to talk while you are eating.
- Try eating smaller meals and having snacks throughout the day.
Try some physical activity
People can find it hard to do physical activity if they have breathlessness. But keeping active can help improve your fitness and can actually help your breathing.
It's best to plan an activity – and then make sure you have breaks and rest periods before you do anything else. For example, if you're going to walk to the shops in the morning, make sure that you can then rest in the afternoon.
Physical activity could include walking, gardening or swimming. Or it could be practising sitting to standing movements, or simply moving your arms and legs in bed.
A physiotherapist can give you a programme of exercises designed just for you. Some hospitals and hospices run exercise groups for patients who are breathless.
These are things to be aware of when you're being physically active:
- You should still be able to talk in short phrases as you exercise. If you cannot do this, slow down until you get your breath back.
- Controlled breathing exercises can help manage your breathing while you exercise.
- Plan ahead for a short walk (for example) by thinking about where there are walls or benches you can use to rest. Planning ahead like this can stop you becoming anxious that you will not be able to find somewhere to stop.
Becoming breathless when you're exercising can be unpleasant but it's not usually harmful and it should settle after you rest for a few minutes.
Walking aids
Some people find that using a walking aid, like a wheeled walker, can help their breathing. This is probably because the way that you lean forward and put pressure on your arms to use the aid helps you to get air into your lungs. And if you're finding it difficult to walk, it can also be a good way to continue to do physical activity that can help with your breathing more generally.
Using a walking aid can also mean you can stop for a rest without having to sit down and get back up again. And if using a walking aid means you can be more mobile this may help with your confidence too.
You can ask your doctor, nurse or physiotherapist about using a walking aid.
Cut down on smoking
Smoking can make breathlessness worse. If you smoke and want support to stop or cut down, ask your doctor or nurse. They can discuss a range of different ways to help you to stop.
Use a fan
A draught of cool air across your face can help you to feel less breathless. You could try using a small hand-held fan. They're cheap and you can carry one around so you have it whenever you need it.
If you're inside, it can help to open a window as long as it's not too cold for you. You could also have a desk fan, or a stand-up fan to create a draught of air in the room. A fan should be put so that the air hits one side of your face just in front of your ear. It can be used alongside breathing exercises to help you slow your breathing rate and recover from an episode of breathlessness more quickly.
Medicines for breathlessness
There are different medicines that can help with breathlessness. Some of them treat the illness that's causing your breathlessness. Some medicines help reduce the feeling of breathlessness. Ask your doctor or nurse about the best medicines for you.
Medicines for an illness causing breathlessness
Medicines that help to reduce the feeling of breathlessness
Complementary therapies
Some people find that complementary therapies like acupuncture, reiki and massage make them feel more relaxed, and this can help with their breathlessness.
Speak to your doctor or nurse before trying complementary therapy. They can advise you on the safety of different types of therapy. Some complementary therapies might not be suitable or safe for you. It will depend on your health condition and treatment.
It's also important to tell the complementary therapist about your medical condition and any treatments that you've had or are having. They can make sure the therapy is suitable for you.
Some complementary therapies are free from the NHS, but they're not always available. Speak to your doctor or nurse about what's available in your area. Your local hospice or a local support group may also offer free or reduced cost therapies. You can also get complementary therapies privately, but you will have to pay for these. Private therapists can be expensive, so it's worth checking the cost first.
Breathlessness diary and action plan
Keeping a diary of the times when you feel breathless can be helpful. It can help you plan activities for times when you have more energy and make the most of the energy that you have.
You may also want to use the action plan. This a place to write down the techniques and medicines that work well for you. Keeping a note of what works well can help you to know what to try next time you feel breathless.
Professionals who can support you
If you need help to manage your breathlessness, there are lots of professionals who can support you. Your GP, hospital team or local hospice will be able to refer you to other professionals.
Breathlessness towards the end of life
Breathlessness can affect people at any stage of their illness. Sometimes someone's breathlessness can get worse as their illness progresses and they near the end of their life.
People can still use the techniques that have helped them before, such as controlled breathing and using a fan, if it's comfortable for them. Sometimes the breathlessness may improve for a while as someone's less able to do activities and has to rest more.
There are medicines that can keep someone comfortable even as they become more breathless. A doctor or nurse can help with medicines if breathlessness becomes more difficult to manage.
Supporting someone with breathlessness
If someone important to you has breathlessness, there are things you can do to support them:
- You might need to take on more tasks like cooking and cleaning. It can help to understand that doing more for them may change your relationship to the person.
- If you need extra help with tasks like cooking and cleaning, speak to the person's doctor, nurse or social worker.
- Talk to the person themselves about what activities are most important for them to do.
- Support them to do those activities at their own pace.
- See if you can help them with breathing exercises and with relaxation techniques.
- Ask if they would like you to go with them to appointments or group sessions where you can learn about breathing control. This might make it easier for you to help them with the techniques.
- Keep rooms well-ventilated by opening windows or using a fan.
- Encourage them to talk about any fears or worries they have.
Supporting someone with breathlessness due to a terminal illness can be rewarding but it can also be very challenging. If you need extra support, speak to your GP about how you're feeling. They can support you with your own health, refer you to a social worker, or recommend support groups in your local area.
Getting support
If you would like to speak to someone, you can call our Marie Curie Support Line for free on 0800 090 2309* or email support@mariecurie.org.uk. Our Support Line can provide emotional support, or they can arrange for you to speak to an Information and Support Nurse if you'd like practical information.
Marie Curie's Online Community may also be a place to connect with others who are living with breathlessness or caring for someone who has this symptom.