Welcome to the blog
Discover the impact of our care on the lives of real people, expert views, celebrity interviews and much more.


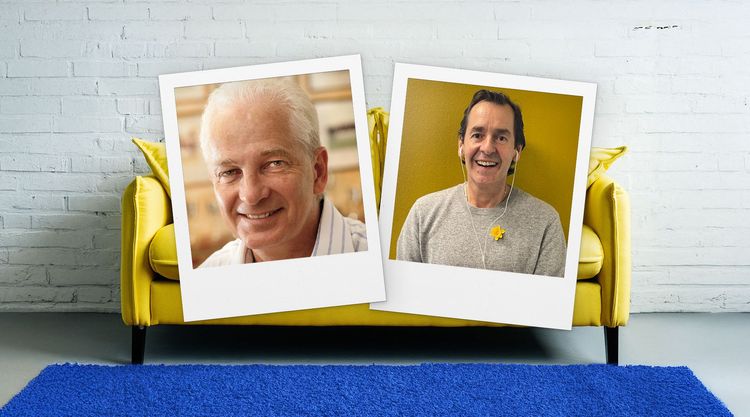
In the latest episode of On the Marie Curie Couch, David Gower OBE sits down with Jason Davidson.
Maria’s been volunteering as a Marie Curie Companion for six years. She explains her role and how it’s changed the way she sees the world.

©2025 Marie Curie. Registered Charity, England and Wales (207994), Scotland (SC038731). Registered company limited by guarantee, England & Wales (507597). Registered Office: One Embassy Gardens, 8 Viaduct Gardens, London SW11 7BW